
I hadn’t realised it was Infertility Awareness Week until I came across another couples NIAW post in my WordPress feed. There’s no reason for me to be aware of it I guess just as World Allergy Week, MS Awareness Week and Bowel Cancer Awareness month have also slipped past me this week. As a Mum of two I’m no longer affected by infertility, I don’t know anyone with Bowel cancer or MS thankfully and none of us suffer from allergies. That wasn’t always the case though – I experienced fertility issues long before my husband and I started trying to conceive. Having now successfully become pregnant and carried babies to full term I wanted to share a little of what that journey has looked like – physically, mentally and emotionally. I’m typing as I’m thinking to ensure I don’t get too hung up on the story being crafted as carefully as my usual blog posts so please forgive me if I jump about or include photos that might seem a bit random to you (they’re not to me) with the purpose of breaking up big chunks of text a little. It’s a long read so feel free to go and make a cuppa first before you settle down. When you reach the end if you know anyone who might feel encouraged by our story please do share the blog link. I’ll also post on Instagram and Twitter if that’s an easier option for you to pass it on.

Our son Euan was born in January 2012, 13 years into our marriage and 10 years after we started trying to conceive. He was a rainbow baby, born 12 days before the first anniversary of the miscarriage of our first baby. I wrote about that experience last year in Writing when you’re lost for words – healing after miscarriage. Both babies were conceived with the help of fertility treatment and Euan was conceived in the first cycle after the miscarriage when our fertility consultant had matter of factly encouraged us to try again as researchers have found that many women are more fertile straight after a miscarriage. The irony of that was not lost on us when my body had taken over a decade to fall pregnant for the first time. We were uncertain where our fertility consultant was unshakeably certain. We’d experienced a deep grief for the baby we’d lost but felt ready to consider the possibility we could fall pregnant again so we out our faith in her when we had no other place for it. We left the fertility clinic with our next supply of Gonal F injections and I clung to the mantra
”When the world says ”Give up”, Hope whispers ”Try one more time”.
 The medical treatment we were receiving was to tackle infertility as a result of PCOS (Polycystic Ovary Syndrome). I had been diagnosed with the condition in 2004 when attempts to fall pregnant naturally had failed because I wasn’t producing any eggs. The agony of waiting month after month for signs of ovulation when you are trying to conceive is stressful enough but my menstrual cycle ranged from 4 months to 9+ months gaps, and no two periods were ever closer than 8 weeks apart. I’d always wondered if only one of my ovaries worked as my cycle had been erratic since my first period at 13. My bleeds were embarrassingly unpredictable but entirely pain free. I didn’t experience the mood swings or PMS symptoms other girls complained about and as an introverted teenager thought how lucky I was to be getting off so lightly.
The medical treatment we were receiving was to tackle infertility as a result of PCOS (Polycystic Ovary Syndrome). I had been diagnosed with the condition in 2004 when attempts to fall pregnant naturally had failed because I wasn’t producing any eggs. The agony of waiting month after month for signs of ovulation when you are trying to conceive is stressful enough but my menstrual cycle ranged from 4 months to 9+ months gaps, and no two periods were ever closer than 8 weeks apart. I’d always wondered if only one of my ovaries worked as my cycle had been erratic since my first period at 13. My bleeds were embarrassingly unpredictable but entirely pain free. I didn’t experience the mood swings or PMS symptoms other girls complained about and as an introverted teenager thought how lucky I was to be getting off so lightly.
It turned out the ease of my menstrual symptoms was due to a hormonal imbalance which affected the frequency with which my body produced eggs. In 2004 the solution offered by the Gynae consultant we were referred to was a prescription for Clomid, an oral medication that is effective for many women in stimulating the ovaries to produce eggs. For some women with ovulation issues taking Clomid for a short period of time is enough to get things working and they fall pregnant naturally. For other women, like me, it has little or no effect at all (I later read in a journal of Chinese Medicine that when egg production ceases as a result of PCOS taking clomid is like flogging a dead horse!). When I say Clomid had no effect I simply mean on helping me to ovulate – it had an extreme effect on my hormonal balance. After a couple of months of taking Clomid I started to suffer menopausal like symptoms like hot flushes, headaches, an increase in appetite, weight gain and raging mood swings. I was effectively suffering an almost constant cycle of PMS without recognising it as that because I’d never had such symptoms before. To be frank I felt like I was unravelling. The stress of all these physical symptoms with no signs of an effect on triggering either ovulation or a bleed, alongside daily monitoring of my basal body temperature and mucus changes was exhausting. Each month when the Clomid failed to work the dose was increased. Each month the Clomid failed to work I became more anxious, depressed and fearful that I’d never be a Mum.
When the World says ”Give up”,
Hope whispers ”Try one more time”
Finally after 6 months, and only one period experienced in that time, we were due to have a review appointment at the hospital. We decided to speak to our kind and supportive GP about our concerns regarding the extreme side effects of Clomid and how it was affecting my mental health. We were worried about documented research that Clomid assisted pregnancies have a higher risk of birth defects and that it’s use is not recommended beyond 6 months. Our GP was sympathetic and said he would certainly caution against continuing to take it even if it was the only option at this stage for helping us to fall pregnant. We left with heavy hearts but encouraged he appreciated the strain treatment was placing on my mental health and recognising that was reason enough to ask further questions.
When we saw the Gynae consultant the following week he suggested another 3 months of Clomid combined with the diabetic drug Metformin as it had been shown to be a successful in many cases where erratic ovulation is a result of PCOS. This is because weight gain is an issue affecting fertility in many PCOS sufferers and this combination of medication is said to help with weightloss. I questioned the rationale of me taking it when I had no other symptoms of being a PCOS sufferer like acne or excess facial hair and only weighed 8.5 stone. The consultant’s reply was ‘‘well you’re lucky then, you’re in the 20% of women who are asymptomatic”. I didn’t feel lucky. I felt alarmed and anxious and fearful about what sort of mother I would be if continuing with treatment that left me feeling unhinged was the only way to drag a baby out of me. We asked the consultant about other options if taking Clomid and Metformin didn’t have the desired effect.
”Unless you opt for donor eggs you’ll never fall pregnant. And you’ll have to pay for it, IVF is not available on the NHS” he answered so matter of factly that I wanted to slap him and scream ‘‘what do you know about women’s bodies anyway!”. Instead I could only swallow down a whisper ”Oh” as I tried not to cry.
I’d always felt something was wrong with me when I noticed my cycle was different to every one elses. I also knew from the moment I started babysitting as a teenager my greatest desire was to become a Mum. When I met George at 19, having a family was not something we talked about straightaway but I fell so hard and fast in love with him that I knew it would be a conversation one day and I wanted reassurance having children would be possible for us. Both my anxious mind and logical brain agreed that only ovulating 2 or 3 times a year would make trying to conceive a frustrating, difficult and potentially depressing journey. We were students in Lancaster and I visited a local GP to express my concerns about my lack of periods. The reply? ”Do you want to fall pregnant right now? Don’t worry about it then, I can prescribe you the pill if you want the reassurance of having a regular period”.
 George and I married in 1998 at the age of 23 and agreed to wait 3 years so that George could set up a recording studio in the cellar in our house and establish his work as a freelance practitioner. We started trying to conceive after 2 years when it became apparent my cycle was not predictable enough to need to worry about falling pregnant sooner. George didn’t feel ready but he was able to deal with his emotions around that better than I was able to manage the depression I was experiencing waiting and watching as other friends became parents so easily. When we then received the news in 2004 that we weren’t going to be able to fall pregnant naturally without risking both my health and our financial future we walked away from the NHS. I wasn’t able to accept such a dim prognosis but we also didn’t have the funds for IVF (having reasoned you can’t start one cycle without knowing you have the resources to keep going if it doesn’t work first, second, third time round). We knew personally of a couple who’d tried numerous IVF cycles over a 10 year period only to be left with a huge debt, a body in constant pain and more damaged than when they started and finally having to accept that they would remain childless. I didn’t feel we’d really received much of a treatment plan at this stage. IVF felt like a last resort not a first resort and using someone elses eggs was also not part of the plan we’d made for creating children together. So instead over the next few years I made dietary changes and tried more holistic, alternative therapies like acupuncture, Chinese herbs, reflexology and EFT for the anxiety and depression that had arisen as a result of the challenges we were dealing with. In that time I had waves of extraordinary optimism and vigour and spells of deep despair. Mostly I just plodded along trying to make day to day life mean something when really life was on hold until we knew for sure whether becoming parents was even possible. When my friends little boy asked me why we didn’t have children I explained it was a bit like making a cake and I didn’t have all the ingredients needed to make a baby. We smiled through the pain of friends announcing their pregnancies and witnessing their family grow by one, two, three children. I answered questions about whether we wanted kids with a conversation killing ”not yet” and cried in private afterwards at my inability to be honest about how I really felt. After a while people stopped asking but that made it no easier to bear to be presumed to be a woman who didn’t want to have children when the opposite was true.
George and I married in 1998 at the age of 23 and agreed to wait 3 years so that George could set up a recording studio in the cellar in our house and establish his work as a freelance practitioner. We started trying to conceive after 2 years when it became apparent my cycle was not predictable enough to need to worry about falling pregnant sooner. George didn’t feel ready but he was able to deal with his emotions around that better than I was able to manage the depression I was experiencing waiting and watching as other friends became parents so easily. When we then received the news in 2004 that we weren’t going to be able to fall pregnant naturally without risking both my health and our financial future we walked away from the NHS. I wasn’t able to accept such a dim prognosis but we also didn’t have the funds for IVF (having reasoned you can’t start one cycle without knowing you have the resources to keep going if it doesn’t work first, second, third time round). We knew personally of a couple who’d tried numerous IVF cycles over a 10 year period only to be left with a huge debt, a body in constant pain and more damaged than when they started and finally having to accept that they would remain childless. I didn’t feel we’d really received much of a treatment plan at this stage. IVF felt like a last resort not a first resort and using someone elses eggs was also not part of the plan we’d made for creating children together. So instead over the next few years I made dietary changes and tried more holistic, alternative therapies like acupuncture, Chinese herbs, reflexology and EFT for the anxiety and depression that had arisen as a result of the challenges we were dealing with. In that time I had waves of extraordinary optimism and vigour and spells of deep despair. Mostly I just plodded along trying to make day to day life mean something when really life was on hold until we knew for sure whether becoming parents was even possible. When my friends little boy asked me why we didn’t have children I explained it was a bit like making a cake and I didn’t have all the ingredients needed to make a baby. We smiled through the pain of friends announcing their pregnancies and witnessing their family grow by one, two, three children. I answered questions about whether we wanted kids with a conversation killing ”not yet” and cried in private afterwards at my inability to be honest about how I really felt. After a while people stopped asking but that made it no easier to bear to be presumed to be a woman who didn’t want to have children when the opposite was true.
Eventually in 2009 after I’d quit a mentally stressful job I took some time out. My anxiety levels normalised, I started to exercise more regularly and for the first time in my life I was able to look after myself properly with no thought for anyone else. When I still had no cycle to speak of after 10 months I felt like we’d tried everything we could naturally and spoke again to the GP who had supported us 5 years before. We admitted it was not an easy decision to return to the NHS but a friend receiving treatment for endometriosis was told she would qualify for free IVF treatment if other interventions didn’t work. Suddenly we had options again and felt it would be important to have a conversation at least with my friend’s new Consultant and find out how fertility treatments had advanced in the last 5 years. We were referred to Mrs Reddy at Gloucestershire Royal Hospital who is a Gynae Consultant and specialist in Reproductive Medicine and was just starting up a new fertility unit in Cheltenham. Mrs Reddy’s response at our first appointment was in complete contrast to our last appointment in 2004. She simply said
‘‘I know what the problem is and we can fix it. I can help you to have a baby, I’ve helped women in much worse situations than you become pregnant. You’re going to be a Mum’’.

Mrs Reddy explained to us why having polycystic ovaries meant I didn’t produce eggs: my ovaries were swollen with hormonal fluid and effectively stuck in the luteal phase of my cycle (the 2 weeks after you ovulate). The fluid filled cysts on my ovaries meant my hormone balance was completely out of balance – neither producing enough leutenizing hormone to produce a viable egg or enough progesterone to trigger a bleed. It was as if my body thought it was pregnant and didn’t need to ovulate without realising it wasn’t! Mrs Reddy then explained she would carry out investigative laparoscopic surgery and and ovarian drilling to release the fluid and reset the hormonal balance. She also said that fertility treatment was now available on the NHS in Gloucestershire and we were eligible for one funded cycle of IVF or 6 cycles of ovulation induction (approximate costs privately of £5,000 and £2,000). I trusted Mrs Reddy completely and that was as valuable in our attempts to prime my body for pregnancy as the vitamins I was taking, the low carb diet I adopted (PCOS effects insulin levels which is why weight gain is an issue for some women) and the positive and hope filled mindset it was now easier to maintain. She’d answered all my questions, had helped me understand the condition that was affecting my fertility and gave me a reason to have faith in my body again because I trusted her skill in unlocking it’s potential. In just one short consultation my faith had been restored in my body, the medical profession and the vision I had always held of being a Mum holding my own baby.
The day after our 12 year wedding anniversary in September 2010 I started the first treatment cycle for ovulation induction. I’d had the laparoscopy and ovarian drilling 5 months before and had experienced intense feelings of excitement and relief that something concrete was finally happening. It still seems surreal to me reflecting back on going into an operation with no fear or worry, only tremors of excitement that finally I was going to be out of the starters blocks on this gruelling infertility journey. It took me 6 weeks to recover fully from the operation and once again we watched and waited for signs of ovulation which never came. My friend with endometriosis had successfully fallen pregnant after her laparoscopy and although that pregnancy had ended in miscarriage she had a baby girl the month after my operation. I was filled with such joy and hope and it was the first pregnancy news in years that hadn’t hurt my heart.
If you’ve not heard of ovulation induction treatment before it involves daily injections of Gonadatrophins, in our case Gonal F, to stimulate your ovaries to produce egg follicles. You need regular scanning of your ovaries once you’ve been injecting for a couple of weeks to see how many egg follicles are growing. It’s the same stimulation process that is used for IVF but the dose is lower and managed more precisely so that only 1 or 2 eggs are produced (in IVF the ovaries are hyper-stimulated and a great many eggs might be extracted). The egg producing follicles on your ovaries are monitored so closely in ovulation induction to avoid the risk of multiple pregnancies as once you ovulate no further medical intervention is needed to conceive or support your pregnancy. When an egg follicle measures 15mm in diameter it is nearly ready to burst so you are given another injection called Ovitrelle to ensure the egg matures and is released. If scanning your ovaries shows more than two follicles have reached 15mm the cycle is suspended and you have to wait to start over again. Thankfully the medical staff know what they’re doing and this doesn’t often happen.
Soon after starting the Gonal F injections I observed in my journal:
”I was apprehensive at first about injecting myself, but unlike George who’s phobic of needles, it’s not any physical worries but simply because it feels like everything hangs on getting this little thing right. I’m sure you can’t get it wrong but it feels so immense to finally be in this place with options. And it’s weird, the enormity of it, to be stood in the kitchen on my own, getting my head around how just 10 seconds of my time has the potential to change everything. George couldn’t even be in the house the first night I injected myself – he texted before returning from badminton to ask if it was all over. I have to inject at the same time every evening so I opted for 10pm just before bed so there was no danger of forgetting (as if I could!). He crept like a cat burglar into the house, panic stricken that I might have felt unable to do it and would need him to now. As it was I had spoken to a friend who’s diabetic and she assured me it was simple and pain free and could be practiced on an orange. It was actually quite mind blowing to think injecting into my belly fat would be the start of making our dreams come true”.
We didn’t conceive following our first cycle of ovulation induction but it was definitely a success story in terms of showing us it was possible. Producing viable eggs was more than I could have ever hoped for – tracking the growth of my follicles on the ultrasound was the tangible evidence that helped us remain hopeful. I felt strangely numb when I got my period after that first cycle, not really disappointed because I’d not allowed myself to imagine we would fall pregnant first time but not really ok about it either. It had taken over 3 weeks of daily injections and visits to the clinic every few days from day 14 for scanning all carried out in secret and fitted in around work for both of us. Once I had ovulated the 2 weeks of waiting had been much harder to bear than I had thought it would be. I’d experienced such intense emotional changes while injecting, was totally fatigued in the latter weeks of the cycle and my boobs had definitely changed! Menstrual symptoms are so similar to pregnancy symptoms I now know but despite what I read I couldn’t bring myself to believe that painful boobs meant I was pregnant. I felt sure that I would know if I was and the ‘Am I?/Arent I?’ conversations in my head were so doubtful I felt sure it meant I wasn’t. You have to let go of any sense of timescale when you’re trying to conceive with help and know that if it takes another month it’s no big deal. Each month takes you closer to, not away from, the child you are dreaming of and with each bleed you can only momentarily mourn an unsuccessful cycle before rejoicing in the start of a new one.
We fell pregnant with our second ovulation induction cycle. We didn’t really let ourselves believe it until we were scanned at 7 weeks and saw our baby’s healthy heartbeat on the screen. We were discharged from the fertility clinic into the care of our local maternity services and one of the first things our Community Midwife arranged for us was our 12 week scan. After wanting to be pregnant for so long the physical difficulties of acid reflux, morning sickness that lasted all day and headaches from not being able to eat or sleep properly hit hard. That pregnancy ended in miscarriage when we were told at our 12 week scan our baby had died at 8 weeks. My body had held on to my baby despite the changes in hormones I’d experienced (only noticeable in my morning sickness suddenly stopping at 10 weeks). We opted for an ERPC procedure to remove the baby as the most complete way of healing physically and emotionally and to ensure fewer risks for achieving future pregnancies.
5 weeks later on 10th March 2011 I wrote in my journal:
”I’ve got out of the habit of journalling which is not a bad thing – it means nothing too awful has happened to write about! I’ve picked up my pencil today because we saw Mrs Reddy yesterday. She gave us her condolences and said how common miscarriage is and that it’s better this way if the pregnancy wasn’t healthy, if there was something not right with the baby. She said that pregnancy hormones take a few weeks to change in the body when a baby dies so the baby’s heart would have stopped beating soon after our first scan since the baby only measured 8 weeks in size. It means my body hung on to our baby for 4 weeks and that’s bitter sweet in terms of the faith I now have in my body’s ability to carry a baby. When I asked if we needed to wait 3 months before commencing treatment (and that George was going away to France for a badminton tournament in couple of months time) she laughed and said ”there’s no medical reason to wait, babies are more important than badminton! You will get pregnant again, I’m sure of it”.
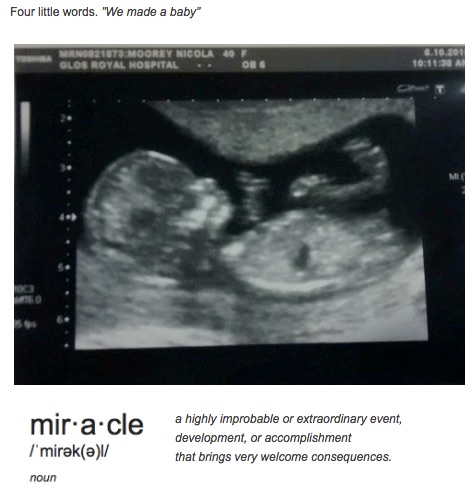
Sure enough in less than 2 months I was pregnant for the second time having successfully matured 2 egg follicles. It was an exciting but tense time wondering whether we would find we were pregnant with twins and when we were scanned again at 7 weeks it was such a relief to see a tiny heartbeat flickering on the screen. We nicknamed our miracle babybird as the baby looked like a little bird on the screen. It was so reassuring to be hearing the news of a healthy baby in a place that had become a second home to us, supported by people we trusted implicitly.
 When we returned to the ultrasound department of our local hospital 5 weeks later for our dating scan it was hard not to feel fretful. George had it worse than me as he had nothing tangible to prove it was going to be ok. I felt certain it was ok though as I felt so sick still, really struggled to drink the litre of water required before the ultrasound and was already started to experience pelvic pain. We were both holding our breath as the Sonographer concentrated on the image on her screen and then turned it towards us asking ”do you want to meet your baby?”. The 20 week scan was an even greater milestone – seeing our baby looking like an image from a pregnancy book was hugely reassuring. The timing couldn’t have been more blessed falling in the same week as what would have been the due date for our first baby.
When we returned to the ultrasound department of our local hospital 5 weeks later for our dating scan it was hard not to feel fretful. George had it worse than me as he had nothing tangible to prove it was going to be ok. I felt certain it was ok though as I felt so sick still, really struggled to drink the litre of water required before the ultrasound and was already started to experience pelvic pain. We were both holding our breath as the Sonographer concentrated on the image on her screen and then turned it towards us asking ”do you want to meet your baby?”. The 20 week scan was an even greater milestone – seeing our baby looking like an image from a pregnancy book was hugely reassuring. The timing couldn’t have been more blessed falling in the same week as what would have been the due date for our first baby.

And that’s where I’m going to stop – stories of pregnancy, birth, and parenting are for another day and another place. Thank you so much for reading this far. I hope that by sharing our experience of a long and painful infertility journey it provides some hope to others that medical professionals do sometimes get it wrong and self-belief and hope is as valuable as practical measures you might take in trying to become parents. Medical professionals can also get it right, dedicate their lives to helping people have children and be amazing in the support they provide. When you understand clearly, as a patient, what the issue is and how it can be overcome it’s much easier to maintain the hope of changing it. (I appreciate for some people fertility issues are unexplained and that brings with it a whole heap of other challenges). For anyone experiencing the pain of being childless there is support to be found in speaking to others about it. If you don’t feel comfortable to do that among your own friends and family an on-line support forum can be a useful place to share your difficulties with people in the same situation, in a way you feel more in control of and less vulnerable about. There is such a silence around difficulties conceiving and the impact it has on living your best life. It’s hard going through treatment in secret or later sharing the pain of losing a baby know one knew existed. But it’s all worth it when the world says ”Give Up” and Hope whispers ‘‘Try one more time” and the result is finally holding your own baby in your arms.

Footnote:
Infertility is a puzzle and what works for some people doesn’t work for others. Who knows what small change is the pivotal moment in completing your picture of becoming a family. Some of the things I feel made a difference for us were:
a proper diagnosis of the medical condition causing our infertility and ensuring we understood what having PCOS meant not only in terms of our fertility issues but also my long term health. With or without a baby PCOS put me at greater risk of other health issues in later life and it made making the diet and lifestyle changes I I needed to make to improve my chances of falling pregnant easier to maintain knowing it was about maintaining good health as a parent.
absolute trust in the knowledge and skill of the medical professionals helping us. When someone says ”You will get pregnant” it’s hard to believe them but if you trust them you can hold faith in them when your own wavers
feeling empowered to do something myself to be as healthy as I could be. By understanding PCOS more and it’s effect on insulin levels I was able to remain more committed to a low sugar/carb diet. I didn’t have weight issues but have since observed that a high carb diet causes bloating, fatigue and low mood which was not helpful in any area of my life on top of struggling with infertility
learning to trust my body and not blame myself for our infertility. This was massive for me having always suffered self-esteem and body confidence issues. The intuition that I had around struggles to fall pregnant in future was accurate but anxiety turned it into questioning my own worth, not being good enough, not deserving happiness etc. Only when I was able to confidently say ”I do deserve to be a Mum. It’s ok to have what I want. It isn’t selfish to put myself first” did something shift in my ability to believe it was possible.
taking vitamin supplements specifically designed to support conception. I wanted to give my body the best possible chance so took Vitabiotics Pregnacare conception vitamins from the month before we started our first cycle of fertility treatment. For the first time in his life George also Pregnacare conception vitamins for men because he also wanted to do everything he could to maximise our chances. I recall he actually said ‘‘if you suffered a miscarriage and I’d been slack about my role in making a healthy baby I’d always wonder if it might have been preventable. I don’t really know if it’ll make a difference but you think it will so I’m not doing to doubt that”.
managing anxiety levels in all areas of my life. My feelings of anxiety about not being able to fall pregnant or sustain a pregnancy were nothing compared to the constant rumbling anxiety I began to experience in the workplace. I didn’t realise until I took a break from paid employment just how badly it was effecting my health. I was underweight because my cortisol levels were so high and I just didn’t have the strategies I needed to manage it because I was wound so tightly. As a result on the rare occasion I shared our difficulties some people would point to my stress levels and say ”You just need to relax and then it’ll happen naturally”. This is never helpful for someone trying to conceive but there is a grain of truth in it; in the need to learn to manage a more positive response to difficult situations. Until I learned to put myself first and respect what my body and mind needed I wonder if there was a psychological block in my body’s ability to create the environment needed to conceive.
exploring the mind body connection and it’s role in fertility issues. I read and worked through a book called The Whole Person Fertility Programme by Neravi Payne in the 5 years between NHS treatments. It was really helpful in unpicking some of the unconscious beliefs I was holding about my ability to fall pregnant, carry a baby and deal with thoughts of coping if we lost a baby. When I was 14 a friend of my Mum’s had suffered a still birth at full term after the heartbreak of multiple miscarriages and committed suicide. Even at that young age I recall vividly feeling her pain and understanding her choice. I think my immature brain converted the idea that miscarriage equals a pain so unbearable you can’t live and wonder if at an emotional level at least my body knew I wasn’t ready to fall pregnant and carry that risk (I’m not saying I would have made that choice of course just acknowledging the connection between body and mind is strong enough to protect us from our own fears sometimes)
having regular acupuncture treatment and using Chinese herbs. The aim initially was to re-balance my body and normalise my cycle but in the end I realised it was actually supporting me at a deeper level than that. Mentally and emotionally I was ragged from so many years of disappointment, was completely disconnected from my body which I felt was failing me and I had so many doubts about what sort of Mum I’d be I needed to restore my faith in myself and find some inner peace that with or without a baby I was ok.
practicing relaxation techniques to manage my anxiety thinking. I’d go for walks to take the lid off my head, had long soaks in the bath and read more books. I was trying to reconnect mind and body and find the still small voice that believed ‘‘it’ll be alright, we can do this, your children are waiting for you”
journalling through the good, bad and sad days. Writing is therapy for me I now realise, sometimes it’s the only way I can tune into the still small voice and quieten the anxious liar.
spending time around family and friends with children. It wasn’t easy, it was painful at times but it was part of the process to learn to be vulnerable with people and let them in. I really believe that tapping into the love you feel for other people’s children and feeling the physical sensation of hugging them, laughing with them and helping them when they’re struggling stirs up your natural parenting instincts. Miracles happen when you open up your heart to others and let joy in.
If you enjoyed this post or know someone who might find encouragement in it I would really appreciate you sharing it with them. Thank you
Wow, what a remarkable journey. Heartbreaking but but then heart lifting. Thank you for sharing this, I have very little knowledge about infertility. I am so pleased that you met Mrs Reddy & what gorgeous children you have xx
Thank you so much. We have lots to be grateful for in the UK where treatment is funded. Euan was made and saved on the NHS after a complicated delivery so we’re doubly thankful. That’s a whole other story for another day ;0)
So pleased you got to have your babies. My sister in law went through similar and has twin baby girls. It is amazing what you can do with the right help xx
Thank you Susan, happy to hear your sister-in-law had successful treatment too. Hoorah for medical advancements and tonnes of hope x
[…] 2018 Footnote: Euan is 6 now and has a 2 year old brother. I’ve finally written the back story to this one to support the aims of National Infertility Awareness Week to break the stigma around fertility issues. Thanks for reading ‘’Our infertility journey through PCOS to parenthood’ […]
WOW WOW WOW! What a powerful story. Thanks for giving me hope through your story. Your babies are beautiful!
Thank you Theresa, we think so too ;o)
Hope whispers but she’s always there to help carry you along when the struggle is deep. Wishing you lots of love and encouragement on your journey to parenthood x
What a journey you have been on,congratulations on your beautiful children #keepingitreal@_karendennis
Thank you Karen, so kind of you to comment. I count my blessings everyday for the gift they are x
What a journey you have been on, I’m so glad you got your dream to have children in the end. I did suffer from secondary infertility but once i got pregnant my body seemed to be kickstarted and I ended up having another 2.
#keepingitreal
Thank you for reading our story and sharing yours. Our bodies are amazing aren’t they. Wow 4 children, that must have been quite the adventure :0)
OMG what a journey you have had and I am so glad it ended happily for you. I am sure your story will inspire many others going through the same experience. Thank you for sharing 🌟 #keepingitreal
Thank you so much for reading and commenting. I still find myself looking at my boys in wonder that they’re really here. I shall never take being their Mum for granted and I really hope that our story provides some cheer and hope to others in a similar season.
Hi Nic, what a journey you went on to get the family you so wanted. I know we should respect Doctors, they only have our best interests at heart, but sometimes I do wonder if they can really relate to their patients (as in a male Dr talking to a woman trying to get pregnant), yes they may know their stuff, but they’ll never know what it’s like to be a woman.
I love that quote about giving up & hope. We naturally hang on to hope, even when it’s slim.
My Auntie struggled with fertility and eventually gave up the idea of ever being a Mum. She fell pregnant naturally at 38 and went on to have two children, sadly she never lived to see them make their way in the world. Very sad.
It’s fantastic that you shared your story. I am sure there are so many women out there going through exactly the same.
Thank you for popping over and linking up with #keepingitreal.
xx
thank you for taking the time to comment Debbie and I appreciate you tweeting my post as part of #keepingitreal. There is something mystical about hope beyond all reason. It’s hard to live with the curve balls life throws out without it. I’m glad your aunty realised her dream of being a Mum even if her time was cut short. It is the hard part of being an older Mum which I try not to dwell on too much!
I havent been blogging for a few years but I remember Euan being born but not the whole back story of the pregnancy and birth, what amazing reading! It was the allotments we had in common at the time., I no longer have mine as all of our circumstances change and we have to go with the flow.
best wishes to yourself and family x
how lovely to hear from you Peggy. I noticed you were no longer blogging when I checked back in a few years after E was born. I’m sorry to hear you don’t have your plot anymore but hope you have some growing space at least, lots you can do in pots and you had a real green thumb as my German relatives would say. Are you going to start blogging again do you think?
[…] 2017 update – these flowers were all sent to me following our miscarriage but at the time I wasn’t able to write that. I have shared our story now in this post https://nipitinthebud.wordpress.com/2017/08/24/writing-lost-for-words-healing-miscarrage/. Please share it with anyone who needs some hope during the dark days and encouragement to believe that their miracle is on it’s way. The back story to our miscarriage is also here – Our infertility journey through PCOS to parenthood […]